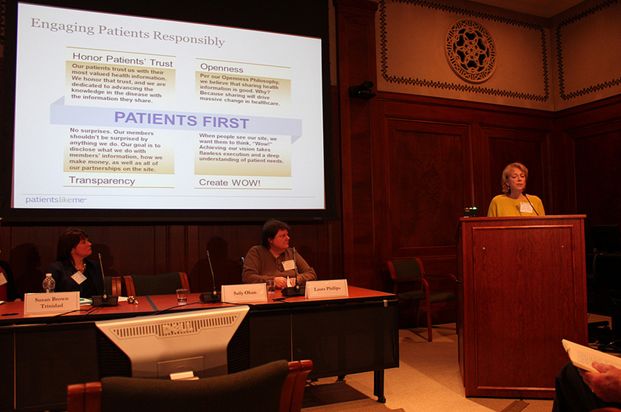
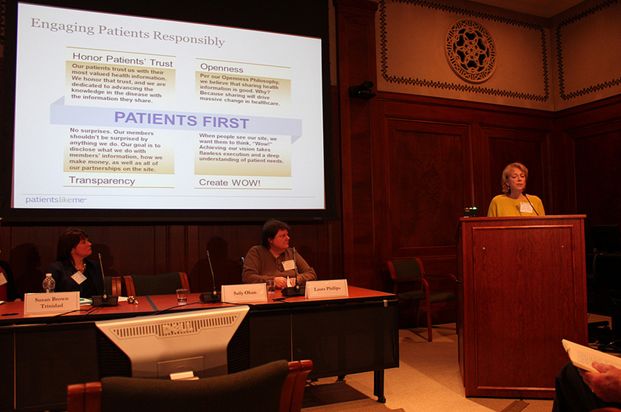
Last week I had the pleasure of attending the Institute of Medicine’s (IOM) Partnering with Patients workshop, where PatientsLikeMe’s Health Data Integrity & Patient Safety Director Sally Okun, RN, MMHS, and PatientsLikeMe member Laura Phillips, who has multiple sclerosis (MS), shared the stage as co-presenters. It was a novel approach to incorporate a patient co-presenter into our presentation, and Sally reported that it made the experience quite special for her.
The day-and-a-half-long meeting brought together clinicians, researchers, policy makers, advocates, patients and caregivers—people who all care about creating better value and improving the quality of healthcare in the US. In the opening remarks by IOM Chairman Michael McGinnis, whose arm was in a sling, we were reminded that everyone is a patient at some point, but most don't always have that mindset.
 The meeting covered many topics, including the problems with healthcare that are complicated and hard to change. Coming from the PatientsLikeMe community team, the topic that struck me most was empowering patients to meaningfully participate in the decisions that affect them, such as which treatment to take or which doctor to see. There are many barriers to finding the answers, and we have a long way to go in making the answers more accessible, but I was happy to reflect on how our growing community of 180,000+ patients is already becoming more involved in their care by sharing their symptom and treatment data with each other.
Here were two other key takeaways from the workshop, as well as a look at how PatientsLikeMe is addressing each issue:
1. Patients need more information – and better information.
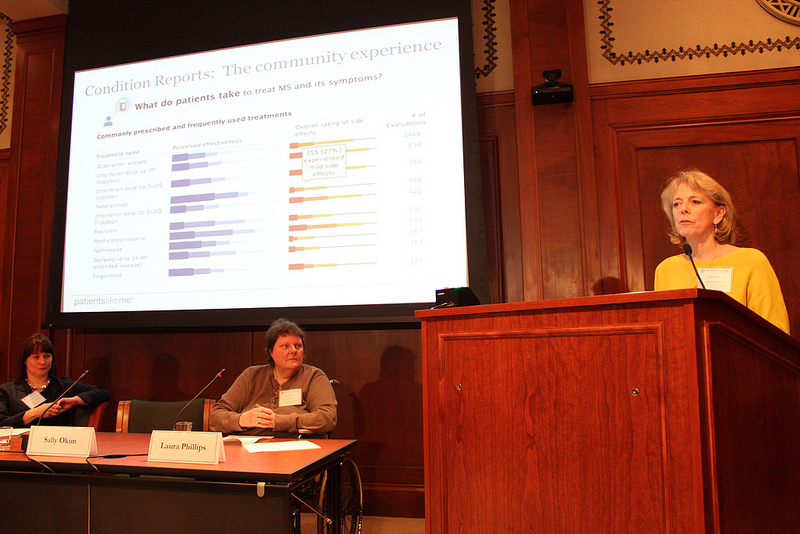
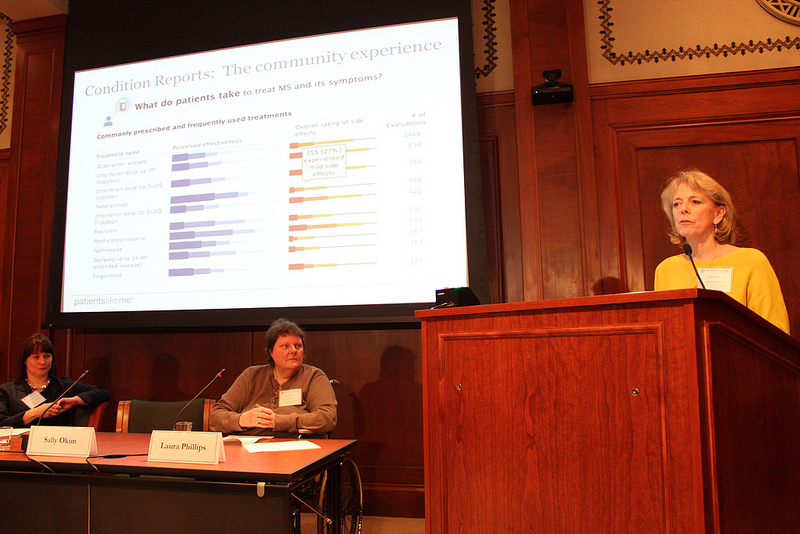
We heard that patients don't have enough information, and they don't know how to use the information they do have. Research articles are convoluted, access is limited, options aren’t presented; and as we heard from rheumatoid arthritis (RA) patient Kelly Young, who writes the blog RA Warrior, textbook definitions may not apply to everyone.
In contrast, our PatientsLikeMe community is sharing what's normal to them, helping others interpret and digest research and creating a real-world database of what is actually going on with their health conditions. That way, members can learn the different treatment options and disease courses, discover the questions they haven’t yet thought about, and decide what's right for them.
The meeting covered many topics, including the problems with healthcare that are complicated and hard to change. Coming from the PatientsLikeMe community team, the topic that struck me most was empowering patients to meaningfully participate in the decisions that affect them, such as which treatment to take or which doctor to see. There are many barriers to finding the answers, and we have a long way to go in making the answers more accessible, but I was happy to reflect on how our growing community of 180,000+ patients is already becoming more involved in their care by sharing their symptom and treatment data with each other.
Here were two other key takeaways from the workshop, as well as a look at how PatientsLikeMe is addressing each issue:
1. Patients need more information – and better information.
We heard that patients don't have enough information, and they don't know how to use the information they do have. Research articles are convoluted, access is limited, options aren’t presented; and as we heard from rheumatoid arthritis (RA) patient Kelly Young, who writes the blog RA Warrior, textbook definitions may not apply to everyone.
In contrast, our PatientsLikeMe community is sharing what's normal to them, helping others interpret and digest research and creating a real-world database of what is actually going on with their health conditions. That way, members can learn the different treatment options and disease courses, discover the questions they haven’t yet thought about, and decide what's right for them.
 2. The entire doctor/patient culture could use a tune-up.
There was a massive call for a “culture change” in many areas of healthcare, including the way clinicians and patients interact. Jeff Belkora from the University of Califormia, San Francisco, and his team of pre-medical interns shared how having an advocate can make a big difference in doctors’ appointments. For example, an advocate can help you define your questions, actually ask them in the office and be an active participant in making decisions about your care.
While some argue the culture change needs to come from both patients and clinicians, PatientsLikeMe members are already taking huge leaps in demanding to be heard. Members are sharing that it’s okay to fire your doctor, learn from others the right questions to be asking and arrive at doctors’ appointments with your own data in hand, including PatientsLikeMe’s handy Doctor Visit Sheet.
Overall, it was great to see so many people focused on making healthcare better, and that all of these various groups are looking to other consumer models for best practices. I truly felt that the workshop attendees were dedicated to listening—and finding new ways to listen—to families and patients in the name of better care.
What did PatientsLikeMe member Laura Phillips think of the IOM workshop? Check out her take.
2. The entire doctor/patient culture could use a tune-up.
There was a massive call for a “culture change” in many areas of healthcare, including the way clinicians and patients interact. Jeff Belkora from the University of Califormia, San Francisco, and his team of pre-medical interns shared how having an advocate can make a big difference in doctors’ appointments. For example, an advocate can help you define your questions, actually ask them in the office and be an active participant in making decisions about your care.
While some argue the culture change needs to come from both patients and clinicians, PatientsLikeMe members are already taking huge leaps in demanding to be heard. Members are sharing that it’s okay to fire your doctor, learn from others the right questions to be asking and arrive at doctors’ appointments with your own data in hand, including PatientsLikeMe’s handy Doctor Visit Sheet.
Overall, it was great to see so many people focused on making healthcare better, and that all of these various groups are looking to other consumer models for best practices. I truly felt that the workshop attendees were dedicated to listening—and finding new ways to listen—to families and patients in the name of better care.
What did PatientsLikeMe member Laura Phillips think of the IOM workshop? Check out her take.

 The meeting covered many topics, including the problems with healthcare that are complicated and hard to change. Coming from the PatientsLikeMe community team, the topic that struck me most was empowering patients to meaningfully participate in the decisions that affect them, such as which treatment to take or which doctor to see. There are many barriers to finding the answers, and we have a long way to go in making the answers more accessible, but I was happy to reflect on how our growing community of 180,000+ patients is already becoming more involved in their care by sharing their symptom and treatment data with each other.
Here were two other key takeaways from the workshop, as well as a look at how PatientsLikeMe is addressing each issue:
1. Patients need more information – and better information.
We heard that patients don't have enough information, and they don't know how to use the information they do have. Research articles are convoluted, access is limited, options aren’t presented; and as we heard from rheumatoid arthritis (RA) patient Kelly Young, who writes the blog RA Warrior, textbook definitions may not apply to everyone.
In contrast, our PatientsLikeMe community is sharing what's normal to them, helping others interpret and digest research and creating a real-world database of what is actually going on with their health conditions. That way, members can learn the different treatment options and disease courses, discover the questions they haven’t yet thought about, and decide what's right for them.
The meeting covered many topics, including the problems with healthcare that are complicated and hard to change. Coming from the PatientsLikeMe community team, the topic that struck me most was empowering patients to meaningfully participate in the decisions that affect them, such as which treatment to take or which doctor to see. There are many barriers to finding the answers, and we have a long way to go in making the answers more accessible, but I was happy to reflect on how our growing community of 180,000+ patients is already becoming more involved in their care by sharing their symptom and treatment data with each other.
Here were two other key takeaways from the workshop, as well as a look at how PatientsLikeMe is addressing each issue:
1. Patients need more information – and better information.
We heard that patients don't have enough information, and they don't know how to use the information they do have. Research articles are convoluted, access is limited, options aren’t presented; and as we heard from rheumatoid arthritis (RA) patient Kelly Young, who writes the blog RA Warrior, textbook definitions may not apply to everyone.
In contrast, our PatientsLikeMe community is sharing what's normal to them, helping others interpret and digest research and creating a real-world database of what is actually going on with their health conditions. That way, members can learn the different treatment options and disease courses, discover the questions they haven’t yet thought about, and decide what's right for them.
 2. The entire doctor/patient culture could use a tune-up.
There was a massive call for a “culture change” in many areas of healthcare, including the way clinicians and patients interact. Jeff Belkora from the University of Califormia, San Francisco, and his team of pre-medical interns shared how having an advocate can make a big difference in doctors’ appointments. For example, an advocate can help you define your questions, actually ask them in the office and be an active participant in making decisions about your care.
While some argue the culture change needs to come from both patients and clinicians, PatientsLikeMe members are already taking huge leaps in demanding to be heard. Members are sharing that it’s okay to fire your doctor, learn from others the right questions to be asking and arrive at doctors’ appointments with your own data in hand, including PatientsLikeMe’s handy Doctor Visit Sheet.
Overall, it was great to see so many people focused on making healthcare better, and that all of these various groups are looking to other consumer models for best practices. I truly felt that the workshop attendees were dedicated to listening—and finding new ways to listen—to families and patients in the name of better care.
What did PatientsLikeMe member Laura Phillips think of the IOM workshop? Check out her take.
2. The entire doctor/patient culture could use a tune-up.
There was a massive call for a “culture change” in many areas of healthcare, including the way clinicians and patients interact. Jeff Belkora from the University of Califormia, San Francisco, and his team of pre-medical interns shared how having an advocate can make a big difference in doctors’ appointments. For example, an advocate can help you define your questions, actually ask them in the office and be an active participant in making decisions about your care.
While some argue the culture change needs to come from both patients and clinicians, PatientsLikeMe members are already taking huge leaps in demanding to be heard. Members are sharing that it’s okay to fire your doctor, learn from others the right questions to be asking and arrive at doctors’ appointments with your own data in hand, including PatientsLikeMe’s handy Doctor Visit Sheet.
Overall, it was great to see so many people focused on making healthcare better, and that all of these various groups are looking to other consumer models for best practices. I truly felt that the workshop attendees were dedicated to listening—and finding new ways to listen—to families and patients in the name of better care.
What did PatientsLikeMe member Laura Phillips think of the IOM workshop? Check out her take.

